📑 Contents
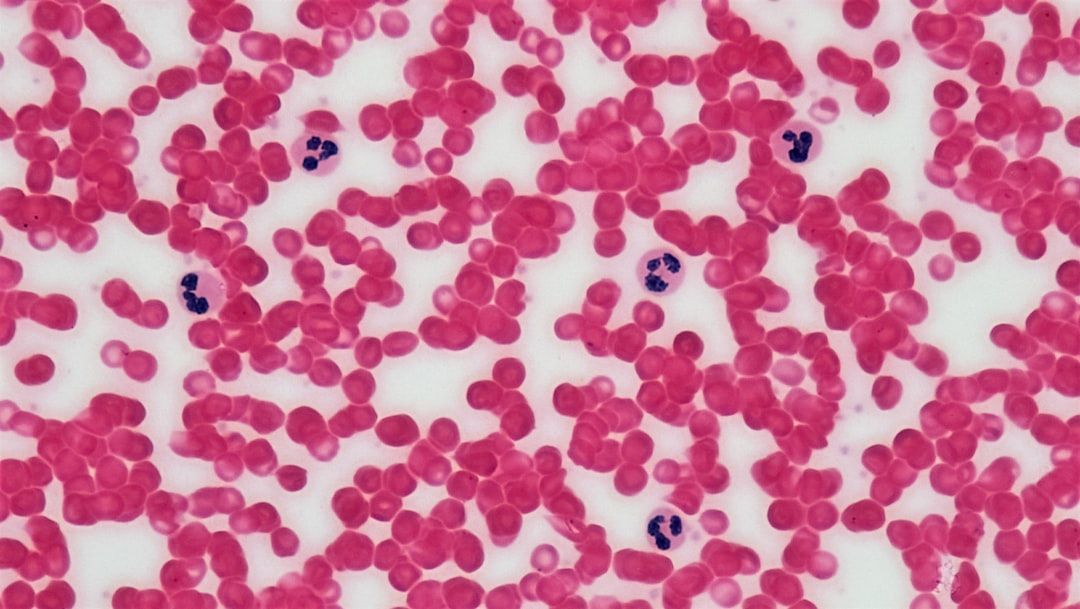
📌 Quick Summary: The future of the hepatitis B vaccine for newborns is uncertain as US advisors consider changing vaccination guidelines.
Hepatitis B Vaccine for Babies Faces Uncertain Future
As we step into the latter part of 2025, the fate of the hepatitis B vaccine for newborns hangs in the balance. A panel of US vaccine advisors is set to vote on a pivotal decision regarding the guidance that mandates all newborns receive the hepatitis B vaccine at birth. This development has sparked discussions not only about public health but also about the broader implications of vaccine research, particularly in the realm of artificial intelligence (AI) and machine learning.
Overview
The hepatitis B virus (HBV) poses significant health risks, particularly in infants and young children. Chronic infection can lead to severe liver complications, including cirrhosis and liver cancer. The hepatitis B vaccine has been a cornerstone of public health strategy since its introduction in the 1980s, significantly reducing the incidence of the disease among vaccinated populations. However, recent debates have emerged over the necessity and efficacy of administering this vaccine at birth. The upcoming vote by the vaccine advisory panel comes in the wake of new data suggesting varying prevalence rates of hepatitis B in the U.S. population, prompting experts to re-evaluate existing vaccination guidelines.
Advocates for the vaccine assert that early vaccination is crucial in preventing HBV transmission, especially in high-risk populations. Conversely, some experts question the blanket policy, arguing for a more nuanced approach based on individual risk factors. This pivotal moment in vaccine policy is not just a matter of public health but also a reflection of the evolving landscape of vaccine research influenced by technological advancements.
📚 Related Articles
Key Details
📚 Related Articles
The discussion surrounding the hepatitis B vaccine is multifaceted. Proponents argue that the vaccine is a safe and effective measure to protect infants from HBV, particularly in cases where mothers are carriers of the virus. In contrast, opponents of the current policy suggest that the prevalence of hepatitis B has decreased significantly and that a one-size-fits-all approach may not be necessary. They advocate for alternative strategies that could focus on screening mothers for HBV and vaccinating only those infants deemed to be at higher risk.
The implications of this vote extend beyond immediate public health concerns. With the rise of digital health technologies, there are questions about how data related to vaccination will be managed and protected. The integration of AI and machine learning in vaccine research has shown promise in enhancing our understanding of vaccine responses and developing new immunization strategies. However, with these advancements come cybersecurity risks, as sensitive health data could be vulnerable to breaches that may compromise vaccine integrity and public trust.
Furthermore, the debate over the hepatitis B vaccine brings to light the larger challenges facing vaccine development today. Public skepticism surrounding vaccines, often exacerbated by misinformation, poses a significant barrier to achieving herd immunity. As vaccine policies evolve, it is essential to address not only the scientific and medical aspects but also the social and ethical dimensions of immunization strategies.
Impact
The potential rescindment of the hepatitis B vaccination guideline for newborns could have far-reaching consequences. If the panel votes to recommend against universal vaccination at birth, it may lead to increased variability in vaccination practices across different states and healthcare providers. This could create disparities in the protection of vulnerable populations, particularly among infants born to mothers with undiagnosed or untreated hepatitis B.
In the broader context, the outcome of this vote may influence how other vaccines are approached in terms of administration schedules and target populations. As healthcare systems grapple with the ramifications of such decisions, there is a pressing need for transparency in the decision-making process. This includes clear communication with the public about the reasons behind vaccine recommendations and their implications for community health.
Moreover, the intersection of technology and vaccine development cannot be overlooked. The innovative use of machine learning in vaccine research has demonstrated potential in predicting vaccine efficacy and identifying optimal formulations. However, if cybersecurity risks are not adequately addressed, the valuable data generated through these processes could be compromised, ultimately undermining public confidence in vaccination efforts.
Insights
As we navigate this uncertain landscape, it is crucial to understand the complexities surrounding vaccine guidelines and their implementation. The discussion around the hepatitis B vaccine for babies highlights the importance of evidence-based decision-making. By harnessing AI and machine learning, researchers can refine vaccine development processes, ensuring that they are responsive to emerging health challenges.
Moreover, it is essential for regulators and policymakers to engage with the public, fostering an environment of trust and understanding. The evolution of vaccine policies must be communicated effectively to counteract misinformation and build community confidence in vaccination programs.
Takeaways
The fate of the hepatitis B vaccine for babies is currently uncertain, with implications that extend beyond public health. As technology continues to shape vaccine research, addressing cybersecurity risks and fostering transparency will be key to maintaining public trust. The upcoming vote signifies a critical juncture in the ongoing dialogue about vaccination strategies and their impact on community health.
🔗 Resources
- World Health Organization (WHO) – Hepatitis B
- Centers for Disease Control and Prevention (CDC) – Hepatitis B Vaccination
- National Institutes of Health (NIH) – Hepatitis B Vaccine Research
- American Academy of Pediatrics (AAP) – Immunization Recommendations
- Vaccine Adverse Event Reporting System (VAERS)
🔗 Resources
- World Health Organization (WHO) – Hepatitis B
- Centers for Disease Control and Prevention (CDC) – Hepatitis B Vaccination
- National Institutes of Health (NIH) – Hepatitis B Vaccine Research
- American Academy of Pediatrics (AAP) – Immunization Recommendations
- Vaccine Adverse Event Reporting System (VAERS)
Conclusion
As the vote on the hepatitis B vaccine for newborns approaches, the stakes have never been higher. The decision will not only influence vaccination practices but will also play a role in shaping the future of public health in the U.S. As we rely more on technological advancements like AI and machine learning in vaccine development, it is imperative to navigate the accompanying challenges—particularly cybersecurity risks. Ultimately, fostering public trust through transparency and evidence-based practices will be crucial in ensuring the continued success of vaccination programs and protecting the health of future generations.